“Drug-Induced/Iatrogenic Dementia: A Perfect Crime”
By all accounts, the woman, in her late 60s, appeared to have severe dementia. She was largely incoherent. Her short-term memory was terrible. She couldn’t focus on questions that medical professionals asked her.
By Judith Graham, KHN News.
But Dr. Malaz Boustani, a professor of aging research at Indiana University School of Medicine, suspected something else might be going on. The patient was taking Benadryl for seasonal allergies, another antihistamine for itching, Seroquel (an antipsychotic medication) for mood fluctuations, as well as medications for urinary incontinence and gastrointestinal upset.
To various degrees, each of these drugs blocks an important chemical messenger in the brain, acetylcholine. Boustani thought the cumulative impact might be causing the woman’s cognitive difficulties.
He was right. Over six months, Boustani and a pharmacist took the patient off those medications and substituted alternative treatments. Miraculously, she appeared to recover completely. Her initial score on the Mini-Mental State Exam had been 11 of 30 — signifying severe dementia — and it shot up to 28, in the normal range.
An estimated 1 in 4 older adults takes anticholinergic drugs — a wide-ranging class of medications used to treat allergies, insomnia, leaky bladders, diarrhea, dizziness, motion sickness, asthma, Parkinson’s disease, chronic obstructive pulmonary disease and various psychiatric disorders.
Older adults are highly susceptible to negative responses to these medications. Since 2012, anticholinergics have been featured prominently on the American Geriatrics Society Beers Criteria list of medications that are potentially inappropriate for seniors.
“The drugs that I’m most worried about in my clinic, when I need to think about what might be contributing to older patients’ memory loss or cognitive changes, are the anticholinergics,” said Dr. Rosemary Laird, a geriatrician and medical director of the Maturing Minds Clinic at Advent Health in Winter Park, Fla.
Here’s what older adults should know about these drugs:
The Basics
Anticholinergic medications target acetylcholine, an important chemical messenger in the parasympathetic nervous system that dilates blood vessels and regulates muscle contractions, bodily secretions and heart rate, among other functions. In the brain, acetylcholine plays a key role in attention, concentration, and memory formation and consolidation.
Some medications have strong anticholinergic properties, others less so. Among prescription medicines with strong effects are antidepressants such as imipramine (brand name Trofanil), antihistamines such as hydroxyzine (Vistaril and Atarax), antipsychotics such as clozapine (Clozaril and FazaClo), antispasmodics such as dicyclomine (Bentyl) and drugs for urinary incontinence such as tolterodine (Detrol).
In addition to prescription medications, many common over-the-counter drugs have anticholinergic properties, including antihistamines such as Benadryl and Chlor-Trimeton and sleep aids such as Tylenol PM, Aleve PM and Nytol.
Common side effects include dizziness, confusion, drowsiness, disorientation, agitation, blurry vision, dry mouth, constipation, difficulty urinating and delirium, a sudden and acute change in consciousness.
Unfortunately, “physicians often attribute anticholinergic symptoms in elderly people to aging or age-related illness rather than the effects of drugs,” according to a research review by physicians at the Medical University of South Carolina and in Britain.
Seniors are more susceptible to adverse effects from these medications for several reasons: Their brains process acetylcholine less efficiently. The medications are more likely to cross the blood-brain barrier. And their bodies take longer to break down these drugs.
Long-Term Effects
In the late 1970s, researchers discovered that deficits in an enzyme that synthesizes acetylcholine were present in the brains of people with Alzheimer’s disease. “That put geriatricians and neurologists on alert, and the word went out: Don’t put older adults, especially those with cognitive dysfunction, on drugs with acetylcholine-blocking effects,” said Dr. Steven DeKosky, deputy director of the McKnight Brain Institute at the University of Florida.
Still, experts thought that the effects of anticholinergics were short-term and that if older patients stopped taking them, “that’s it — everything goes back to normal,” Boustani said.
Concerns mounted in the mid-2000s when researchers picked up signals that anticholinergic drugs could have a long-term effect, possibly leading to the death of brain neurons and the accumulation of plaques and tangles associated with neurodegeneration.
Since then several studies have noted an association between anticholinergics and a heightened risk of dementia. In late June, this risk was highlighted in a new report in JAMA Internal Medicine that examined more than 284,000 adults age 55 and older in Britain between 2004 and 2016.
The study found that more than half of these subjects had been prescribed at least one of 56 anticholinergic drugs. (Multiple prescriptions of these drugs were common as well.) People who took a daily dose of a strong anticholinergic for three years had a 49% increased risk of dementia. Effects were most pronounced for people who took anticholinergic antidepressants, antipsychotics, antiepileptic drugs and bladder control medications.
These findings don’t constitute proof that anticholinergic drugs cause dementia; they show only an association. But based on this study and earlier research, Boustani said, it now appears older adults who take strong anticholinergic medications for one to three years are vulnerable to long-term side effects.
Preventing Harm
Attention is now turning to how best to wean older adults off anticholinergics, and whether doing so might improve cognition or prevent dementia.
Researchers at Indiana University’s School of Medicine hope to answer these questions in two new studies, starting this fall, supported by $6.8 million in funding from the National Institute on Aging.
One will enroll 344 older adults who are taking anticholinergics and whose cognition is mildly impaired. A pharmacist will work with these patients and their physicians to take them off the medications, and patients’ cognition will be assessed every six months for two years.
The goal is to see whether patients’ brains “get better,” said Noll Campbell, a research scientist at Indiana University’s Regenstrief Institute and an assistant professor at Purdue University’s College of Pharmacy. If so, that would constitute evidence that anticholinergic drugs cause cognitive decline.
The second trial, involving 700 older adults, will examine whether an app that educates seniors about potential harms associated with anticholinergic medications and assigns a personalized risk score for dementia induces people to initiate conversations with physicians about getting off these drugs.
Moving patients off anticholinergic drugs requires “slow tapering down of medications” over three to six months, at a minimum, according to Nagham Ailabouni, a geriatric pharmacist at the University of Washington School of Pharmacy. In most cases, good treatment alternatives are available.
Advice For Older Adults
Seniors concerned about taking anticholinergic drugs “need to approach their primary care physician and talk about the risks versus the benefits of taking these medications,” said Shellina Scheiner, an assistant professor and clinical geriatric pharmacist at the University of Minnesota.
Don’t try stopping cold turkey or on your own. “People can become dependent on these drugs and experience withdrawal side effects such as agitation, dizziness, confusion and jitteriness,” Ailabouni said. “This can be managed, but you need to work with a medical provider.”
Also, “don’t make the assumption that if [a] drug is available over the counter that it’s automatically safe for your brain,” Boustani said. In general, he advises older adults to ask physicians about how all the medications they’re taking could affect their brain.
Finally, doctors should “not give anticholinergic medications to people with any type of dementia,” DeKosky said. “This will not only interfere with their memory but is likely to make them confused and interfere with their functioning.”
July 18, 2019
______________________________________________________________________________
Kris Kristofferson’s Dramatic Cure of his “Incurable” Alzheimer’s Disease
Another Iatrogenic Illness Unveiled
The term “iatrogenic” means doctor, drug or surgery-caused disease. It is a taboo subject in America today.
I don’t know how many of my readers listen to John Gilbert’s daily talk show on Duluth’s local KDAL radio station (610 AM). John is the journalist that writes the best sports-related columns that I have ever read. This morning (8-16-16), just before I was about to begin writing this week’s column, John called and asked me to appear on the show to give my medical opinion about the dramatic recovery of dementia victim Kris Kristofferson, the legendary singer/song-writer who had been erroneously diagnosed with incurable late-stage Alzheimer’s dementia (of unknown origin).
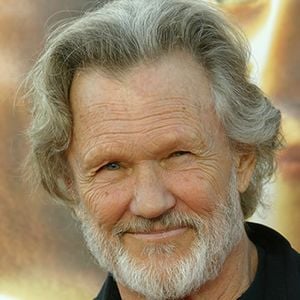 John had seen Kristofferson perform onstage with Merle Haggard a year or two ago when he was obviously seriously demented (although still able to remember the lyrics of his own songs). And then, just recently, John again saw Kristofferson perform in a solo concert when his dementia symptoms had completely disappeared! Reader publisher and editor Bob Boone graciously provided the $70 dollar tickets for John and his wife Joan.
John had seen Kristofferson perform onstage with Merle Haggard a year or two ago when he was obviously seriously demented (although still able to remember the lyrics of his own songs). And then, just recently, John again saw Kristofferson perform in a solo concert when his dementia symptoms had completely disappeared! Reader publisher and editor Bob Boone graciously provided the $70 dollar tickets for John and his wife Joan.
Apparently Kristofferson (right) had been mis-diagnosed with Alzheimer’s dementia about three years ago, which started more than one medical misadventure for he and his neurologists involving neurotoxic medication trials with drugs. Those drugs that Kristofferson was treated with had been approved by the FDA on the basis of a couple of short-term trials involving only a few hundred so-called “Alzheimer’s Dementia” patients. The results that were submitted to the FDA showed only minimal improvement (albeit “statistically significant”), but only in mild to moderate dementia. Thus treating severely demented patients with those drugs was not FDA-approved (“off-label”).
Kristofferson had thus been treated with what is actually now considered by the medical community to be ineffective, non-curative and the cause of many serious drug-induced adverse effects. In other words, Kristofferson a victim of serious dementia and a resident of Big Pharma-dominated America, was given the standard Alzheimer’s drug treatment: oral Namenda (Novartis) and Exelon (Forest Pharmaceuticals, Inc). Another drug that is similar to Namenda is Aricept (Eisai Pharmaceuticals), which has been found to be equally ineffective.
All three of those drugs are highly profitable synthetic drugs that are non-specific anti-cholinesterase drugs that are now actually widely acknowledged to be useless for any kind of dementia – not to mention the fact that they are all very expensive and carry serious and sometimes debilitating adverse effects which can include somnolence, insomnia, fatigue, appetite suppression, dizziness, depression, confusion, emotional lability, fainting, and even diarrhea!
John Gilbert and I are both Kris Kristofferson fans. We both appreciate his song-writing genius (and performances). In my opinion, his lyrics and tunes rank right up there with Bob Dylan, although Kris was more understandable when performing. Some of my favorite Kristofferson songs that come to mind include Me and Bobby McGee, Loving Her Was Easier, Why Me Lord, Sunday Morning Coming Down, Once More With Feeling, Help Me Make it Through the Night, Jody and the Kid, etc.). At the most recent concert that the Gilberts attended, it was revealed that the singer’s so-called (and mis-diagnosed) Alzheimer’s Disease has been miraculously cured three weeks after he stopped three offending drugs and started antibiotic treatment because he had been found to have a positive blood test for Lyme Disease.
Thus, with a new diagnosis that explained a number of his symptoms, Kristofferson’s new physician stopped the two Alzheimer’s drugs and an (unnamed) antidepressant drug that had been prescribed for so-called fibromyalgia, and he was simultaneously started on a tetracycline antibiotic and an anti-protozoal drug (that was FDA-approved only for protozoal diarrheas, such as could occur from giardiasis).
Within three weeks of stopping the medications and starting the antibiotics, Kristofferson’s dementia had improved dramatically. Not surprisingly, all of the glory has been attributed to the new diagnosis and the antibiotic, rather than to the stoppage of the likely offending drugs, which are all known to commonly cause symptoms that could have caused his dementia or fibromyalgia or depression symptoms (see list above)!
According to Kristofferson’s wife (in an interview widely available online),
For the past three years, Kris was treated for Alzheimer’s by two different neurologists. He was on two drugs for it, Namenda and Exelon patches. But finally, a spinal tap and functional MRI ruled out Alzheimer’s, so he quit those meds and the antidepressant for fibromyalgia. They also tested him for Lyme Disease in the spinal fluid and it was negative but the doctor explained to me that Lyme does not live in fluid, it lives in tissue. It bores into tissue so you would really have to do a biopsy of the brain to find it.
He was taking all these medications for things he doesn’t have, and they all have side effects. After he gave up his Alzheimer’s and depression pills and went through three weeks of Lyme disease treatment, all of a sudden he was back.
As mentioned, all the news has been glorifying the new diagnosis of Lyme disease and the antibiotics. The news has also been inadvertently discrediting the doctrinal assertions of the many Alzheimer’s Disease patient advocacy groups (such as the Alzheimer’s Association and the Alzheimer’s Foundation of America [and even the Mayo Clinic’s website]) which state that there are no known causes of AD and consistently fail to mention the many drug-induced (iatrogenic) causes of dementia. The term “iatrogenic” means doctor, drug or surgery-caused disease. It is a taboo subject in America today.
Dementia and Iatrogenesis
At this point it is essential to point out that the epidemic of dementia and mental illness and autoimmune disorders in American adults coincides perfectly with the aggressive prescribing of psychiatric drugs, statin (cholesterol-lowering) drugs and the regular use of mercury (in the annual flu shots) and aluminum adjuvants in the vaccines given to adults, adolescents and children (and infants in many cases). Both mercury and aluminum are toxic to the brains and nerve tissues of all animals, including humans, and statin drugs like Lipitor have FDA-required black box warnings because they are known to cause memory loss, the first and essential symptom of dementia.
A major problem behind America’s over-diagnosing, over-prescribing and over-vaccinating is the fact that there are so many corporate-funded groups with serious economic and/or professional conflicts of interest that work hard to promote the awareness and de-stigmatization of any and every disease for which there is an FDA-approved drug. The corporate sponsors, who have very deep pockets, are everywhere where potential prescribers and potential patients are, and not just on prime time television and the internet.
Some Groups That Promote Over-Diagnosis, Over-Treatment and Over-Vaccination
That list of conflicted groups includes 1) pharmaceutical corporations that sell drugs and vaccines, 2) medical device manufacturers that want to sell their medical devices, 3) diagnostic testing corporations that manufacture and promote their products, 4) Big Vaccine corporations that promote mandatory or mandated vaccination schedules (including unproven-for-safety combination inoculations for infants), 5) patient advocacy groups that promote certain diseases, 6) government bureaucracies that are heavily subsidized by Big Pharma (CDC, FDA, NIH, HHS, etc) and 7) those Big Pharma-connected organizations (AMA, AAP, APA, AAFP, etc) that try to demonize and discredit safer and potentially curative non-drug approaches to ill health like psychotherapy, nutritional therapies, etc.
Actually curing patients or preventing illnesses naturally – rather than treating symptoms with drugs that typically cause adverse effects – is not necessarily good for the healthcare business. (There is a big difference between early diagnosis and primary prevention. The first is highly profitable and the second one isn’t.)
The dramatic Kristofferson story was well-received by the Lyme Association of America and the many similar Lyme patient advocacy groups. However, it has not been well-received by the Alzheimer’s Association because it revealed one of the AA’s blind spots: that there is such a thing as drug-induced dementia that could potentially be cured by stopping the offending drug(s).
“Drug-Induced/Iatrogenic Dementia: A Perfect Crime”
But the whole Kristofferson story raises a number of issues.
For example, one must ask how prevalent is iatrogenic memory loss secondary to prescribed drugs? That is an issue that, if brought up among civilized people with no profit motives, would terrify the thousands of for-profit healthcare corporations and their sycophants.
I have written about psychiatric drug-induced dementia in the past, mainly referring to the ground-breaking book on the subject that is titled “Drug-Induced Dementia: A Perfect Crime”, authored by practicing psychiatrist Grace E. Jackson.
In her scholarly book (which, not surprisingly, has been black-listed by the Big Pharma-influenced medical community because it tells too many unwelcome truths about Big Psychiatry and Big Pharma), Dr Jackson has methodically evaluated the vast basic neuroscience journal literature (most of which has not been subsidized by Big Pharma [as opposed to virtually all mainstream medical journals]). In her studies, Dr Jackson found a massive amount of information proving that all five classes of psychiatric drugs are fully capable of causing brain impairment and brain damage in lab animals (and even human subjects) that mimic findings in dementia patients. And that includes the classical findings of neurofibrillary tangles and beta amyloid deposits. (FYI, the five classes of psychiatric drugs are psychostimulants, antidepressants, tranquilizers/sleeping pills, antipsychotics and mood stabilizers/anti-seizure drugs.)
The Fine Line Between “Normal”, Demented and “Mentally Ill”
The truth is that people diagnosed as “mentally ill” for life are often simply those unfortunates who have found themselves in acute or chronic states of potentially reversible crises or temporary “overwhelm” due to any number of preventable, treatable and even curable situations. Examples include such things as being in bad company, or being a victim of poverty, abuse, violence, torture, homelessness, discrimination, underemployment, malnutrition, addictions/withdrawal, electroshock “therapy” and/or exposure to neurotoxic chemicals in their food, air, water or prescription bottles. Any of those examples can mimic a so-called “mental illness of unknown cause” or a reversible dementia like Kris Kristofferson had.
Those labeled as the “mentally ill” are not much different from those of us who call ourselves “normal”. But we “normals” have just been lucky enough to have not yet decompensated because of some yet-to-happen, desperation-inducing life situation. And thus we may not have yet been given a billable diagnosis with a billable code number, and so we have not yet been prescribed some unaffordable prescription drug that could put us on the road to permanent dependence, disability and institutionalization.
In other words, if we are lucky enough to remain unlabeled, we are also likely to remain off brain-altering and addictive substances; and therefore we may remain away from the clutches of “the system”, within which it is very difficult to “just say no to drugs.”
My clinical experience with over a thousand so-called “mentally ill” patients (most of whom were mis-labeled) has led me to agree with Jackson’s assertions. I fully agree with her warnings that the chronic use of psychiatric drugs is a major cause of memory loss, dementia, cognitive disorders, loss of IQ points, loss of creativity, loss of impulse control, loss of spirituality, loss of empathy, loss of energy, loss of strength, and a multitude of metabolic adverse effects (like psych drug-induced obesity, hypertension, diabetes and hypercholesterolemia).
There is no question in my mind that these drugs can sicken the body, brain and soul by causing adverse drug effects such as insomnia, somnolence, increased depression, mania, anxiety, delusions, psychoses, paranoia, etc. So before filling the prescription, I strongly urge pill-takers to read the product insert information under WARNINGS, PRECAUTIONS, ADVERSE EFFECTS, CONTRAINDICATIONS, TOXICOLOGY, OVERDOSAGE and the ever-present BLACK BOX WARNINGS ABOUT SUICIDALITY, HOMICIDALITY AND MEMORY LOSS.
Dr. Peter Breggin has warned us in his writings about a new syndrome that he calls psychiatric drug-induced Chronic Brain Impairment (CBI). It is caused by the chronic usage, especially with large doses or with combinations of psychotropic drugs. CBI could also be regarded as a chemically traumatic brain injury (cTBI) and it can mimic Alzheimer’s Disease.
In medical school, we students half-joked that Thorazine and Haldol caused “chemical lobotomies” in its victims. Little did we know how close to the truth we were. Chemical lobotomy is a useful way to conceptualize the serious issue CBI or cTBI, because such brain-altered patients are often indistinguishable from those who have actually suffered a physically traumatic brain injury (TBI) or have been subjected to “ice-pick” lobotomies (which were popular in the 1940s and 50s before the drugs came on the market and rapidly replaced that dastardly industry).
America has a dementia and mental ill health epidemic on its hands that is so obvious but so grossly misunderstood, and because of that blindness, the epidemic is worsening, not because of the supposed progression of “mental illness”, but because of the continued chronic use of neurotoxic, non-curative drugs that are, in America, erroneously used as first-line “treatment.”
In conclusion, I attach a number of useful items that support some of the realities mentioned above.
- The CDC, much to the delight of Big Vaccine corporations, spent more than $4 billion in 2015 purchasing childhood vaccines from them.
- The CDC has paid out more than $3 billion to families because of the harm, including deaths and permanent disabilities, caused by certain childhood vaccines.
- Big Pharma’s profit-driven model plays a very significant role in the way public health policy is determined. The power of Big Pharma is not a secret, nor is it a conspiracy theory.
- It is estimated that errors from medical treatment kill up to 98,000 people in U.S. hospitals every year and characterized the problem as among the nation’s leading causes of death and injury.
- Iatrogenic infections in the US (“iatrogenic” — meaning “induced by a physician,” or, more loosely, “caused by medical care”) are directly responsible for 20,000 deaths among hospital patients in the U.S. each year, and they contribute to an additional 70,000 deaths, according to the CDC. The dollar cost of iatrogenic infections is $4.5 billion.
- A new poll from the American Medical Association nonprofit National Patient Safety Foundation (NPSF) finds that 42 percent of people say they’ve been affected by physician errors, either directly or through a friend or relative. The survey found that 40 percent of the people who had experienced a medical mistake pointed to misdiagnoses and, therefore, wrong treatments as the problem. Medication errors accounted for 28 percent of mistakes. AMA leaders say it’s time to bring the issue out into the open, rather than living in constant fear that any admission of error will launch a flood of malpractice lawsuits. Poorly designed health care systems may be largely to blame. Doctors and nurses often work double shifts, making them more prone to error.
Dr Kohls is a retired physician who practiced holistic, non-drug, mental health care for the last decade of his family practice career. He now writes a weekly column for the Reader Weekly, an alternative newsweekly published in Duluth, Minnesota, USA.

